据《自然》杂志网络版近日报道,来自美国埃默里大学神经学家Helen S. Mayberg领导的研究小组发现,通过刺激大脑深处部位,深度抑郁症患者的病情能够得到缓解甚至逆转。首个安慰剂对照研究显示,植入电极刺激疗法的治疗效果可以长期维持。该研究结果发表在最近的《Archives Of General Psychiatry》上。
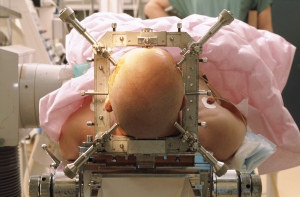
Helen S. Mayberg领导的研究小组在10位抑郁症患者和7位躁郁症患者的大脑胼胝体下扣带回白质中植入电极装置,并对他们进行追踪观察。他们同时还精心设计了适当的安慰剂对照临床研究:患者被告知,电极植入手术完成后他们会立即被随机分配到两个治疗组,其中一个小组将马上接受刺激治疗,另一个小组则在四周后才开始接受刺激治疗,而事实上在此期间没有人接受电极刺激。结果表明,这些患者都没有表现出显著的安慰剂效应(即假药效应,指病人虽获得无效的治疗,但却预料或相信治疗有效,从而让症状得到舒缓的现象)。
有12位患者完成了为期两年的深部脑刺激疗程,除一人之外,其他人都已经完全摆脱了抑郁症困扰或者仅表现出轻微症状。对于习惯看到严重抑郁症患者在施以抗抑郁药物或认知疗法后无法维持治疗效果的精神病医生而言,这一结果近乎奇迹。
Mayberg说:“我们在研究中发现,很多患者在头几个月并没有好转,但经过一年或时间更久的刺激治疗之后,他们开始作出反应。”她表示,躁郁症患者也与抑郁症患者一样有反应,这尤其令研究人员感到高兴,因为躁郁症是出了名的难以治疗,而目前几乎所有的深部脑刺激研究都只针对抑郁症。
但Mayberg格同时也指出,深部脑刺激无法根治抑郁症,一旦停止电极刺激,患者很快又会全面陷入抑郁状态。而且这种方法也不是治疗抑郁症的速战速决之道,因为它不仅涉及侵入性的脑外科手术,恢复过程通常也非常缓慢。
第三阶段涵盖数百名病人的安慰剂对照临床试验现正由两家电极制造商在北美和欧洲的多个研究中心展开,但研究结果要好几年后才能出来。
与此同时,脑深部刺激疗法也将在梅贝格和其他小组的学术研究基础上进行必要的微调。“过去10年来的巨大突破之一就是认识到抑郁症是一种大脑网络疾病。”德国波恩大学精神病专家托马斯·施莱普费说,深部脑刺激就是对大脑不同区域之间表现不佳的网络施以电击,胼胝体下扣带回和伏隔核都是这一网络的一部分,他也曾见过5位接受伏隔核部位接受刺激的抑郁症病人显示出长期疗效,“但我们仍在寻找这一网络上的最佳目标,以帮助(病人)更快地恢复”。

Subcallosal Cingulate Deep Brain Stimulation for Treatment-Resistant Unipolar and Bipolar Depression
Paul E. Holtzheimer, MD; Mary E. Kelley, PhD; Robert E. Gross, MD, PhD; Megan M. Filkowski, BA; Steven J. Garlow, MD, PhD; Andrea Barrocas, MA; Dylan Wint, MD; Margaret C. Craighead, BA; Julie Kozarsky, BA; Ronald Chismar, RN; Jared L. Moreines, BS; Klaus Mewes, PhD; Patricio Riva Posse, MD; David A. Gutman, MD, PhD; Helen S. Mayberg, MD
Context Deep brain stimulation (DBS) may be an effective intervention for treatment-resistant depression (TRD), but available data are limited.
Objective To assess the efficacy and safety of subcallosal cingulate DBS in patients with TRD with either major depressive disorder (MDD) or bipolar II disorder (BP).
Design Open-label trial with a sham lead-in phase.
Setting Academic medical center.
Patients Men and women aged 18 to 70 years with a moderate-to-severe major depressive episode after at least 4 adequate antidepressant treatments. Ten patients with MDD and 7 with BP were enrolled from a total of 323 patients screened.
Intervention Deep brain stimulation electrodes were implanted bilaterally in the subcallosal cingulate white matter. Patients received single-blind sham stimulation for 4 weeks followed by active stimulation for 24 weeks. Patients then entered a single-blind discontinuation phase; this phase was stopped after the first 3 patients because of ethical concerns. Patients were evaluated for up to 2 years after the onset of active stimulation.
Main Outcome Measures Change in depression severity and functioning over time, and response and remission rates after 24 weeks were the primary efficacy end points; secondary efficacy end points were 1 year and 2 years of active stimulation.
Results A significant decrease in depression and increase in function were associated with chronic stimulation. Remission and response were seen in 3 patients (18%) and 7 (41%) after 24 weeks (n = 17), 5 (36%) and 5 (36%) after 1 year (n = 14), and 7 (58%) and 11 (92%) after 2 years (n = 12) of active stimulation. No patient achieving remission experienced a spontaneous relapse. Efficacy was similar for patients with MDD and those with BP. Chronic DBS was safe and well tolerated, and no hypomanic or manic episodes occurred. A modest sham stimulation effect was found, likely due to a decrease in depression after the surgical intervention but prior to entering the sham phase.
Conclusions The findings of this study support the long-term safety and antidepressant efficacy of subcallosal cingulate DBS for TRD and suggest equivalent safety and efficacy for TRD in patients with BP.
文献链接:https://archpsyc.ama-assn.org/cgi/content/abstract/archgenpsychiatry.2011.1456v1








