研究人员用干细胞再生的脑细胞去替换帕金森症中死亡的脑细胞,这一类细胞被移植到猴子大脑中,是朝着帕金森症新疗法的方向迈出重要一步。
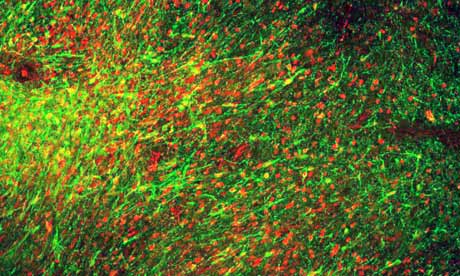
干细胞转化的脑神经元被植入到猴子的大脑中
美国研究人员称:“他们已成功解决掉之前的难题:诱导胚胎肝细胞分化成因帕金森症杀死的神经细胞。实验表明,这些神经细胞在动物体中存活和正常工作,并能扭转帕金森症猴的运动障碍。”
这项突破增加了新疗法的希望:把分泌多巴胺的新细胞移植到病人中,用于治疗帕金森症。
纽约斯隆.凯特琳癌症中心的Lorenz Studer 博士称:“之前,我们不能完全了解特定信号,它告诉干细胞如何分化成特定类型的细胞。”
他还说:“我们以前诱导的细胞能分泌一些多巴胺,但事实上,它们并不是真正的神经细胞,因此,在动物实验中治疗效果很有限。现在,我们知道如何正确诱导,这一点有望用于将来的临床治疗。”
帕金森症发病时,部分大脑黑质中多巴胺分泌细胞会凋亡,引起发抖、僵硬和行动迟缓,有些病人也可能遭受疲倦、疼痛、抑郁和便秘,随着病情的加重,这些病状会加剧。
药物是帕金森症的主要疗法,通过提高多巴胺水平,让它运输到大脑并刺激大脑中多巴胺效应区,最终用于控制症状。一些病人的大脑被植入电极,接受电脉冲刺激用于缓解运动障碍。
大约十年间,科学家一直试图为神经退行性疾病(如,帕金森症和阿尔茨海默氏症)再生神经元,但是,小鼠干细胞分化多巴胺神经细胞的实验不能成功应用于人体,此外还有安全忧虑:人体干细胞分化出多巴胺神经元,这一信号能促发癌症的形成。因此,人体的临床实验尚未开始。
Studer博士和他的同事发现,特定的化学信号需要用于诱导干细胞分化成能分泌多巴胺的正确类型的大脑细胞。相关的研究发表在《Nature》期刊上。
在一系列实验中,按每次不少于1百万个细胞的量,研究小组共注射6次到帕金森症动物的大脑中。这些神经元在小鼠、大鼠和猴子病理模型中存活、搭建新连接以及修复失去的运动机能,却没有肿瘤生成的迹象。在实验中猴子病状的改善很重要,因为啮齿动物的大脑需要较少的神经元就可缓解病状。
英国帕金森研究所的主任Kieran Breen称:“干细胞有望治疗和一些帕金森症病人,但是,我们需要确信移植神经元能正常工作。”
他还说:“研究人员已经可以诱导人体干细胞分化成正确类型的神经元,它们能分泌帕金森症患者缺少的化学物质多巴胺,但是,这些细胞移植到帕金森症动物模型后继续生长,有的转化成肿瘤细胞,问题就会出现。”(生物探索译)
相关英文论文摘要:
Dopamine neurons derived from human ES cells efficiently engraft in animal models of Parkinson’s disease
Human pluripotent stem cells (PSCs) are a promising source of cells for applications in regenerative medicine. Directed differentiation of PSCs into specialized cells such as spinal motoneurons or midbrain dopamine (DA) neurons has been achieved. However, the effective use of PSCs for cell therapy has lagged behind. Whereas mouse PSC-derived DA neurons have shown efficacy in models of Parkinson’s disease, DA neurons from human PSCs generally show poor in vivo performance. There are also considerable safety concerns for PSCs related to their potential for teratoma formation or neural overgrowth. Here we present a novel floor-plate-based strategy for the derivation of human DA neurons that efficiently engraft in vivo, suggesting that past failures were due to incomplete specification rather than a specific vulnerability of the cells. Midbrain floor-plate precursors are derived from PSCs 11 days after exposure to small molecule activators of sonic hedgehog (SHH) and canonical WNT signalling. Engraftable midbrain DA neurons are obtained by day 25 and can be maintained in vitro for several months. Extensive molecular profiling, biochemical and electrophysiological data define developmental progression and confirm identity of PSC-derived midbrain DA neurons. In vivo survival and function is demonstrated in Parkinson’s disease models using three host species. Long-term engraftment in 6-hydroxy-dopamine-lesioned mice and rats demonstrates robust survival of midbrain DA neurons derived from human embryonic stem (ES) cells, complete restoration of amphetamine-induced rotation behaviour and improvements in tests of forelimb use and akinesia. Finally, scalability is demonstrated by transplantation into parkinsonian monkeys. Excellent DA neuron survival, function and lack of neural overgrowth in the three animal models indicate promise for the development of cell-based therapies in Parkinson’s disease.
英文论文链接: https://www.nature.com/nature/journal/vaop/ncurrent/full/nature10648.html







