英国和加拿大等国研究人员在新一期英国医学刊物《柳叶刀》上报告说,局部晚期前列腺癌患者应该在激素疗法的基础上再使用放射疗法,这可以有效地提高患者的生存率。
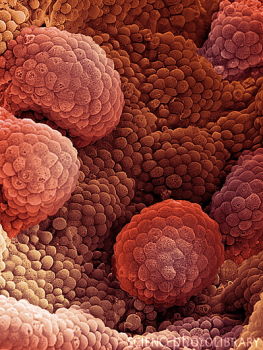
电镜下的前列腺癌
研究人员对1205名局部晚期前列腺癌患者进行了随机对比研究,其中约一半患者采用传统的激素疗法,其余患者则在激素疗法的基础上还使用了放射疗法。随后研究人员对这些患者进行了平均6到7年的跟踪,结果显示,两种疗法都采用的患者生存率明显更高。
英国医学研究委员会的马修·希德斯说,这项研究结果令人鼓舞,因为它不仅显示在激素疗法基础上增加放射疗法有效,并且因为增加放射疗法而带来的副作用是有限的。
男性前列腺癌常与雄性激素有关,因此常用药物控制雄性激素来帮助治疗,这就是激素疗法。而放射疗法用x射线来杀死癌变组织,是常用于治疗各类癌症的一种方法。最近连续有研究显示前列腺癌治疗中应联合使用这两种疗法。但对于局部晚期前列腺癌患者来说,之前一直不清楚联合使用两种疗法对他们是否有效果,本次研究为这个问题给出了肯定结果。
相关英文论文摘要:
Combined androgen deprivation therapy and radiation therapy for locally advanced prostate cancer: a randomised, phase 3 trial
Background Whether the addition of radiation therapy (RT) improves overall survival in men with locally advanced prostate cancer managed with androgen deprivation therapy (ADT) is unclear. Our aim was to compare outcomes in such patients with locally advanced prostate cancer.
Methods Patients with: locally advanced (T3 or T4) prostate cancer (n=1057); or organ-confined disease (T2) with either a prostate-specific antigen (PSA) concentration more than 40 ng/mL (n=119) or PSA concentration more than 20 ng/mL and a Gleason score of 8 or higher (n=25), were randomly assigned (done centrally with stratification and dynamic minimisation, not masked) to receive lifelong ADT and RT (65—69 Gy to the prostate and seminal vesicles, 45 Gy to the pelvic nodes). The primary endpoint was overall survival. The results presented here are of an interim analysis planned for when two-thirds of the events for the final analysis were recorded. All efficacy analyses were done by intention to treat and were based on data from all patients. This trial is registered at controlledtrials.com as ISRCTN24991896 and Clinicaltrials.gov as NCT00002633.
Results Between 1995 and 2005, 1205 patients were randomly assigned (602 in the ADT only group and 603 in the ADT and RT group); median follow-up was 6·0 years (IQR 4·4—8·0). At the time of analysis, a total of 320 patients had died, 175 in the ADT only group and 145 in the ADT and RT group. The addition of RT to ADT improved overall survival at 7 years (74%, 95% CI 70—78 vs 66%, 60—70; hazard ratio [HR] 0·77, 95% CI 0·61—0·98, p=0·033). Both toxicity and health-related quality-of-life results showed a small effect of RT on late gastrointestinal toxicity (rectal bleeding grade >3, three patients (0·5%) in the ADT only group, two (0·3%) in the ADT and RT group; diarrhoea grade >3, four patients (0·7%) vs eight (1·3%); urinary toxicity grade >3, 14 patients (2·3%) in both groups).
Interpretation The benefits of combined modality treatment—ADT and RT—should be discussed with all patients with locally advanced prostate cancer.
Funding Canadian Cancer Society Research Institute, US National Cancer Institute, and UK Medical Research Council.
英文论文链接:https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(11)61095-7/fulltext







