匹兹堡儿童医院John G. Rangos高级研究中心和匹兹堡大学医学院的研究人员识别出一种强效的分子途径,可用于调控肝脏中的胰岛素和新血糖合成。该发现提供了针对糖尿病的新治疗方案,并发表在本周的《Diabetes》期刊上。
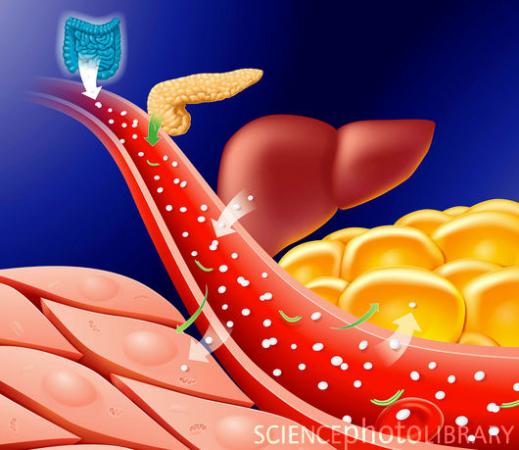
II型糖尿病血糖代谢图
H. Henry Dong博士称:“通常情况下,肝脏会把过量的血糖储存在糖元中,在睡眠和空腹时,小部分糖元可被释放用于让血糖维持在正常生理范围内,但是,即便用胰岛素治疗,糖尿病患者的肝脏仍然会泵出血糖。”
他还说,科学家试图发现能引起肝脏过量合成血糖的因素,如果这些途径被控制住,我们能够减少糖尿病患者体内异常的高血糖水平。
他和研究小组一直研究Forkhead(或称为 FOX)蛋白家族,目前的研究集中在FOX06蛋白上。基因工程小鼠合成过量的FOX06,就会形成糖尿病前兆的代谢综合症,包括在空腹和血糖耐受受损时血糖和胰岛素的高水平。然而,FOX06合成量过低的小鼠在空腹时具有异常低的血糖水平。
其它实验表明,糖尿病小鼠的肝脏中FOX06水平异常得高。尽管血糖没有完全正常化,阻断该蛋白的表达可显著地降低肝脏中血糖的合成。治疗2周内,糖尿病小鼠的血糖代谢出现明显地改善。
人类肝细胞测验证实了FOX06在血糖合成过程中的重要性。
这一发现有力地表明,FOX06有望成为治疗的靶点。如果抑制它的活性,我们能降低糖尿病患者肝脏中血糖的合成,进而能更好地控制血糖水平。(生物探索译 Pobee)
相关英文论文摘要
Forkhead Box O6 Integrates Insulin Signaling With Gluconeogenesis in the Liver
OBJECTIVE Excessive endogenous glucose production contributes to fasting hyperglycemia in diabetes. This effect stems from inept insulin suppression of hepatic gluconeogenesis. To understand the underlying mechanisms, we studied the ability of forkhead box O6 (FoxO6) to mediate insulin action on hepatic gluconeogenesis and its contribution to glucose metabolism.
RESEARCH DESIGN AND METHODS We characterized FoxO6 in glucose metabolism in cultured hepatocytes and in rodent models of dietary obesity, insulin resistance, or insulin-deficient diabetes. We determined the effect of FoxO6 on hepatic gluconeogenesis in genetically modified mice with FoxO6 gain- versus loss-of-function and in diabetic db/db mice with selective FoxO6 ablation in the liver.
RESULTS FoxO6 integrates insulin signaling to hepatic gluconeogenesis. In mice, elevated FoxO6 activity in the liver augments gluconeogenesis, raising fasting blood glucose levels, and hepatic FoxO6 depletion suppresses gluconeogenesis, resulting in fasting hypoglycemia. FoxO6 stimulates gluconeogenesis, which is counteracted by insulin. Insulin inhibits FoxO6 activity via a distinct mechanism by inducing its phosphorylation and disabling its transcriptional activity, without altering its subcellular distribution in hepatocytes. FoxO6 becomes deregulated in the insulin-resistant liver, accounting for its unbridled activity in promoting gluconeogenesis and correlating with the pathogenesis of fasting hyperglycemia in diabetes. These metabolic abnormalities, along with fasting hyperglycemia, are reversible by selective inhibition of hepatic FoxO6 activity in diabetic mice.
CONCLUSIONS Our data uncover a FoxO6-dependent pathway by which the liver orchestrates insulin regulation of gluconeogenesis, providing the proof-of-concept that selective FoxO6 inhibition is beneficial for curbing excessive hepatic glucose production and improving glycemic control in diabetes.







