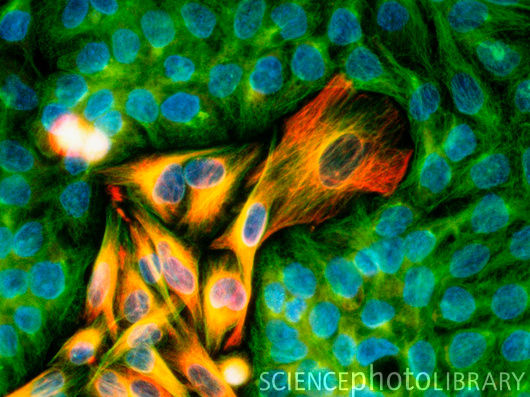
黑色素瘤的免疫荧光图片(图)
据最新研究报道,密歇根州大学肿瘤研究中心的科学家们证实了前哨淋巴结活检能够安全有效的检测出脑部及颈部黑素瘤的扩散及癌变情况。
该活检方法通过注射一种特异性染料来检测肿瘤容易发生扩散的第一个结点。如果检测结果为阴性,病人可以避免进行淋巴结移除手术,以减少不必要的手术打击。如果检测结果显示细胞正发生癌变,病人则可以马上进行放疗、化疗等临床治疗手段。
在此之前,因为脑部和颈部拥有大量关键性的神经和血管,很多外科医生相信前哨淋巴结活检非常的不安全,结果也不准确。
这项研究的论文发表在了最新一期的《Cancer》杂志上,科学家们对353例头部和颈部有黑素瘤的病人在密歇根州大学进行了长达10年的前哨淋巴结活检实验。研究的病人数据显示,除了一个病例外,所有的前哨淋巴结活检均能正确定位,并且该活检没有对任何病人造成永久性的精神损伤。
其中有大约20%的病人被检测出至少有一个前哨淋巴结发生癌变,随后科学家们均进行了淋巴结切除手术。
在剩余的检测结果呈阴性的283例病人中,有12例病人的结果呈现假阳性。这意味着该项检测的误差率仅有4%,这个数据和在身体其它部位检测黑素瘤癌变的活检结果误差率类似。
论文的第一作者,密歇根州大学耳鼻喉学主任Carol Bradford博士说道:“我们对病人的研究结果显示,前哨淋巴结活检对于检测脑部和颈部的黑素瘤恶化癌变是一种安全有效的方法。和检测身体其它的部分一样,脑部和颈部的活检同样安全可行,而且更重要的是它能为患者进行早期的诊断有助于后续的治疗。” (生物探索 Jun译)
生物探索推荐英文论文原文摘要:
Sentinel lymph node biopsy is accurate and prognostic in head and neck melanoma
BACKGROUND:
Sentinel lymph node biopsy (SLNB) has emerged as a widely used staging procedure for cutaneous melanoma. However, debate remains around the accuracy and prognostic implications of SLNB for cutaneous melanoma arising in the head and neck, as previous reports have demonstrated inferior results to those in nonhead and neck regions. Through the largest single-institution series of head and neck melanoma patients, the authors set out to demonstrate that SLNB accuracy and prognostic value in the head and neck region are comparable to other sites.
METHODS:
A prospectively collected database was queried for cutaneous head and neck melanoma patients who underwent SLNB at the University of Michigan between 1997 and 2007. Primary endpoints included SLNB result, time to recurrence, site of recurrence, and date and cause of death. Multivariate models were constructed for analyses.
RESULTS:
Three hundred fifty-three patients were identified. A sentinel lymph node was identified in 352 of 353 patients (99.7%). Sixty-nine of the 353 (19.6%) patients had a positive SLNB. Seventeen of 68 patients (25%) undergoing completion lymphadenectomy after a positive SLNB result had at least 1 additional positive nonsentinel lymph node. Patients with local control and a negative SLNB failed regionally in 4.2% of cases. Multivariate analysis revealed positive SLNB status to be the most prognostic clinicopathologic predictor of poor outcome; hazard ratio was 4.23 for SLNB status and recurrence-free survival (P < .0001) and 3.33 for overall survival (P < .0001).
CONCLUSIONS:
SLNB is accurate and its results are of prognostic importance for head and neck melanoma patients.







