据8月10日刊《美国医学会杂志》上的一则研究披露,睡眠呼吸紊乱的老年妇女(显示有缺氧症)会比那些没有罹患这种疾病的妇女更容易出现认知功能损害或痴呆症。
加州大学旧金山分校的Kristine Yaffe, M.D.及其同事对多导睡眠图(是在睡眠中对生理活动的监测)所测得的普遍存在的睡眠呼吸紊乱与之后的轻度认知功能损害和痴呆症的诊断之间的关系进行了检查。该研究包括了298名在研究开始的时候没有罹患痴呆症的妇女(其平均年龄为82.3岁);她们在2002年1月和2004年4月间的一个骨质疏松性骨折研究的亚组研究中接受了整晚的多导睡眠图检查。睡眠呼吸紊乱被定义为每小时睡眠时的睡眠呼吸暂停-低通气指数为15或以上。睡眠呼吸暂停-低通气指数是在每小时的睡眠中发生呼吸完全停止(无呼吸)和呼吸部分阻塞(呼吸不足)的次数。这些人的认知状态(正常、痴呆或轻度的认知损害)是根据在2006年11月至2008年9月间所收集的资料确定的。研究人员对这些人的缺氧症、睡眠片断化以及睡眠持续时间进行了测量以调查它们在睡眠呼吸紊乱与认知功能损害之间所存在的任何联系的基础机制。
在这298名妇女中,有35.2%的人符合睡眠呼吸紊乱的诊断标准。在对其经过平均4.7年的跟踪之后,这些妇女中有35.9%的人发生了轻度的认知功能损害或痴呆症(轻度认知功能损害:20.1%;痴呆症:15.8%)。有47位罹患普遍存在的睡眠呼吸紊乱的妇女(占44.8%)发生了轻度的认知功能损害或痴呆症,而没有睡眠呼吸紊乱的妇女的这一数字为31.1%。对这些数据的分析表明,睡眠呼吸紊乱的存在与随后出现的轻度认知功能损害或痴呆症几率的增加有关。
研究人员写道:“鉴于在老年人中的睡眠呼吸紊乱和认知功能损害的发生率都很高,这两种病况间存在关系--即使是不太大--的可能性都可能对公众健康产生重大影响。此外,缺氧症--而非睡眠片断化或时间不足--看来与发生轻度认知功能损害或痴呆症有关的发现为人们提供了睡眠呼吸紊乱可能促发认知功能损害的机制的相关线索。认知功能损害与睡眠呼吸紊乱风险增加有关的发现开启了一条对发生轻度认知损害或痴呆症风险进行另外的研究,以及对以包括睡眠呼吸紊乱的睡眠质量作为治疗标靶的预防性策略进行探索的新的通路。”
生物探索推荐英文论文摘要:
Sleep-Disordered Breathing, Hypoxia, and Risk of Mild Cognitive Impairment and Dementia in Older Women
ABSTRACT
Context Sleep-disordered breathing (characterized by recurrent arousals from sleep and intermittent hypoxemia) is common among older adults. Cross-sectional studies have linked sleep-disordered breathing to poor cognition; however, it remains unclear whether sleep-disordered breathing precedes cognitive impairment in older adults.
Objectives To determine the prospective relationship between sleep-disordered breathing and cognitive impairment and to investigate potential mechanisms of this association.
Design, Setting, and Participants Prospective sleep and cognition study of 298 women without dementia (mean [SD] age: 82.3 [3.2] years) who had overnight polysomnography measured between January 2002 and April 2004 in a substudy of the Study of Osteoporotic Fractures. Sleep-disordered breathing was defined as an apnea-hypopnea index of 15 or more events per hour of sleep. Multivariate logistic regression was used to determine the independent association of sleep-disordered breathing with risk of mild cognitive impairment or dementia, adjusting for age, race, body mass index, education level, smoking status, presence of diabetes, presence of hypertension, medication use (antidepressants, benzodiazepines, or nonbenzodiazepine anxiolytics), and baseline cognitive scores. Measures of hypoxia, sleep fragmentation, and sleep duration were investigated as underlying mechanisms for this relationship.
Main Outcome Measures Adjudicated cognitive status (normal, dementia, or mild cognitive impairment) based on data collected between November 2006 and September 2008.
Results Compared with the 193 women without sleep-disordered breathing, the 105 women (35.2%) with sleep-disordered breathing were more likely to develop mild cognitive impairment or dementia (31.1% [n = 60] vs 44.8% [n = 47]; adjusted odds ratio [AOR], 1.85; 95% confidence interval [CI], 1.11-3.08). Elevated oxygen desaturation index (≥15 events/hour) and high percentage of sleep time (>7%) in apnea or hypopnea (both measures of disordered breathing) were associated with risk of developing mild cognitive impairment or dementia (AOR, 1.71 [95% CI, 1.04-2.83] and AOR, 2.04 [95% CI, 1.10-3.78], respectively). Measures of sleep fragmentation (arousal index and wake after sleep onset) or sleep duration (total sleep time) were not associated with risk of cognitive impairment.
Conclusion Among older women, those with sleep-disordered breathing compared with those without sleep-disordered breathing had an increased risk of developing cognitive impairment.
KEYWORDS: aging, anoxia, cognition disorders, dementia, risk factors, sleep apnea syndromes, women's health.
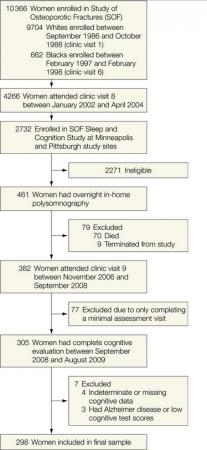
Figure. Progression of Patients Through the Study of Osteoporotic Fractures' Sleep and Cognition Study
生物探索推荐英文原文报道:
Sleep-Disordered Breathing May Increase Risk of Cognitive Impairment, Dementia Among Older Women
Older women with sleep-disordered breathing, as indicated by measures of hypoxia (oxygen deficiency), were more likely to develop cognitive impairment or dementia than women without this disorder, according to a study in the August 10 issue of JAMA.
"Sleep-disordered breathing, a disorder characterized by recurrent arousals from sleep and intermittent hypoxemia, is common among older adults and affects up to 60 percent of elderly populations. A number of adverse health outcomes including hypertension, cardiovascular disease, and diabetes have been associated with sleep-disordered breathing," according to background information in the article. Cognitive impairment also has been linked to sleep-disordered breathing in some studies, but the design of most of these studies has limited the ability to draw conclusions regarding this association. "Given the high prevalence and significant morbidity associated with both sleep-disordered breathing and cognitive impairment in older populations, establishing whether a prospective association exists between sleep-disordered breathing and cognition is important. This is especially important because effective treatments for sleep-disordered breathing exist."
Kristine Yaffe, M.D., of the University of California, San Francisco, and colleagues examined the association between prevalent sleep-disordered breathing as measured with polysomnography (monitoring of physiological activity during sleep) and subsequent diagnoses of mild cognitive impairment and dementia. The study included 298 women without dementia at the beginning of the study (average age, 82.3 years) who had overnight polysomnography measured between January 2002 and April 2004 in a substudy of the Study of Osteoporotic Fractures. Sleep-disordered breathing was defined as an apnea-hypopnea index of 15 or more events per hour of sleep. The apnea-hypopnea index is the number of complete cessations (apnea) and partial obstructions (hypopnea) of breathing occurring per hour of sleep. Cognitive status (normal, dementia, or mild cognitive impairment) was based on data collected between November 2006 and September 2008. Measures of hypoxia, sleep fragmentation, and sleep duration were investigated as underlying mechanisms for any association between sleep-disordered breathing and cognitive impairment.
Among the 298 women, 35.2 percent met criteria for sleep-disordered breathing. After an average of 4.7 years of follow-up, 35.9 percent of the women developed mild cognitive impairment or dementia (mild cognitive impairment: 20.1 percent; dementia: 15.8 percent). Forty-seven women (44.8 percent) with prevalent sleep-disordered breathing developed mild cognitive impairment or dementia compared with 31.1 percent of those without sleep-disordered breathing. Analysis of the data indicated that the presence of sleep-disordered breathing was associated with an increased odds of subsequent mild cognitive impairment or dementia.
The researchers also found, after adjusting for various demographic risk factors, that two measures of hypoxia (an oxygen desaturation index of 15 or greater and a high percentage of total sleep time [greater than 7 percent] in apnea or hypopnea) were associated with higher incidence of mild cognitive impairment or dementia. "Measures of sleep fragmentation (arousal index and wake after sleep onset) or sleep duration (total sleep time) were not associated with risk of cognitive impairment." The authors add that their finding that sleep-disordered breathing was associated with an increased risk of cognitive impairment seems to be related primarily to measures of hypoxia.
"Given the high prevalence of both sleep-disordered breathing and cognitive impairment among older adults, the possibility of an association between the 2 conditions, even a modest one, has the potential for a large public health impact. Furthermore, the finding that hypoxia and not sleep fragmentation or duration seems to be associated with risk of mild cognitive impairment or dementia provides clues to the mechanisms through which sleep-disordered breathing might promote cognitive impairment. The increased risk for cognitive impairment associated with sleep-disordered breathing opens a new avenue for additional research on the risk for development of mild cognitive impairment or dementia and exploration of preventive strategies that target sleep quality including sleep-disordered breathing," the researchers write.
They add that to fully evaluate the impact of treatment for sleep-disordered breathing in elderly populations, additional trials with larger sample sizes, longer treatment periods, and more diverse populations are required. "Of interest, our findings suggest a potential role for supplemental oxygen therapy for sleep-disordered breathing in elderly individuals; however, its role requires critical evaluation in intervention studies."
Editorial: Sleep-Disordered Breathing and Cognitive Decline in Older Adults
In an accompanying editorial, Nicola Canessa, Ph.D., of the Center for Cognitive Neuroscience, and Luigi Ferini-Strambi, M.D., of the Universita Vita-Salute San Raffaele, Milan, Italy, write that "the study by Yaffe et al and related studies to date suggest that large trials with continuous positive air pressure (CPAP) treatment in elderly participants with sleep-disordered breathing should be performed."
"Moreover, in trials evaluating the effects of pharmacological and nonpharmacological (e.g., cognitive training and rehabilitation) interventions on cognitive function in patients with mild cognitive impairment or dementia, the possible coexistence of sleep-disordered breathing should be considered. Finally, physicians of patients with mild cognitive impairment and sleep-disordered breathing for whom treatment with CPAP may be indicated should consider these results, and future guidelines to formalize the clinical management of patients with mild cognitive impairment should consider the implications of this study and related research."







