最新发表在《自然》杂志上的一篇文章称,英国科学家首次成功地将小鼠心脏中的一种具有干细胞特性的细胞——祖细胞转换成心肌,从而证明了成体心脏中存在可重新激活的休眠性修复细胞,经刺激后能够生成心肌,修复受损心脏。
祖细胞又称前体细胞,它居于干细胞和成体细胞之间。与能分化成各种类型细胞的干细胞不同,祖细胞的分化方向已比较确定,通常只能分化成特定类型的细胞。心脏祖细胞在胚胎阶段能够转化成包括心肌细胞在内的一系列特殊细胞。但在成体心脏中,这种转换功能消失了。科学家们认为,这种细胞在成体心脏中依然具有转化功能,恢复其功能就可起到修复心脏的作用。
英国伦敦大学学院的研究人员使用一种叫做Tβ4的蛋白,成功地恢复了成年小鼠心脏中祖细胞在胚胎阶段所具有的转化功能。他们在小鼠心脏受损后,向小鼠体内注射Tβ4加强剂,不仅成功地刺激祖细胞转换成新的心肌,还使其与原有的健康心肌很好地结合起来。
动物实验显示,如果对实验鼠每天注射这种蛋白质,持续一周就可以使其心脏中的祖细胞活力增强。这时如果人为使实验鼠的一些心肌细胞坏死,出现类似心脏病的症状,则祖细胞会逐渐聚拢在受损部位,形成新的细胞,替换掉受损细胞。而对于另一些没有注射这种蛋白质的实验鼠来说,其心脏受损后就没有出现这种自我修复现象。
研究人员称,这一研究表明,恢复祖细胞的转化功能是修复受损心脏的一种可行方式,这对未来心脏疾病的治疗将产生重要影响。但由于使用Tβ4仅能生成少量心肌细胞,因此用这种方法治疗受损心脏或许还需要数年时间。他们正计划进行更深入研究,希望找出更有效的方法激活祖细胞的转化潜力,并最终将此种方法成功用于人体治疗。
编辑圈点:
心脏健康的挽回与补救,乃横亘于世界医疗卫生发展道路上的高墙藩篱之一。尽管替代材料与器械在不断进步,却始终无法比拟肌体的“原装”效果,是以本次探索无论成功与否,其思路都值得嘉许。而在科学技术令人造工艺日臻精密发达的今天,更应回首关注和发掘人体自身的力量,以实现对各类疾病在病理与哲学意义上的双重征服,并让更多的人去理解:我们自身的进化功能,才是人类改造自然能力不断进化延伸的源泉之所在。
生物探索推荐英文原文
Stem cells patch up 'broken' heart
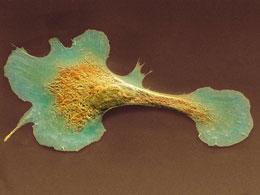
Cardiomyocytes cannot repair themselves after heart attacks.
Cell reactivation in mouse hearts repairs muscle after heart attack.
Time might be enough to heal a heartbreak, but an injured heart can rarely repair itself. However, a study published today inNature reports that a natural protein can activate stem cells in mouse hearts to replace damaged tissue with new muscle cells.
Heart muscle cells, or cardiomyocytes, are irreparably damaged by heart attack. For the heart to continue functioning properly, the damaged cells must be replaced. Heart progenitor cells — cells that can form the various tissues that make up the heart, such as blood vessels and muscle — do exist, but in adults are not active enough to repair damage. So Paul Riley at University College London Institute of Child Health and his colleagues have found a way to wake them up.
Riley and his team used a small protein called thymosin β4 (Tβ4), which is found in many tissues and regulates cell structure and mobility. They had already shown that Tβ4 can induce heart progenitor cells to produce new blood vessels. This time, they were looking for new muscle.
Express delivery
"We studied the activity of a gene called Wt1, because we know that embryonic stem cells expressing Wt1 can become cardiomyocytes, but Wt1 is switched off in adults," says Riley. He and his team injected mice with Tβ4 every day for a week, then anaesthetized the animals and stitched together one of their arteries, mimicking a heart attack. Mice survive this procedure, making it possible to study the way their hearts respond to treatment.
The researchers examined the hearts of mice at various time points after the operation. They found heart cells expressing Wt1 just two days after the injury. The cells were initially in the heart's outer layer, but by two weeks after surgery they had moved inside and clustered around the site of the injury. The cells had also changed in size and shape, and looked just like cardiomyocytes.
Riley and his team are still working out exactly how Tβ4 switches stem-cell genes in the heart cells back on, but they're betting on an epigenetic effect — a chemical change to DNA that affects gene expression. They think that the injury provides a trigger for the stem cells to go ahead and divide, making healthy new muscle cells. The researchers are also trying to work out what that injury signal actually is.
Maurice van den Hoff, a cardiac biologist at the Heart Failure Research Center in Amsterdam who was not involved in the study, says that lipid or bone-marrow stem cells have been used in heart-attack patients before, but that these stem cells don't make true cardiomyocytes, so they won't work in patients long-term. "But heart stem cells are much more likely become the right cell type, and lead to lasting repair," he says.
Wear and repair
Riley thinks that Tβ4, or another molecule of similar effect, might become a daily preventative treatment for people who have a family history of heart disease, much as cholesterol-lowering drugs and anti-clotting agents have done. But Deepak Srivastava, a cardiac stem-cell biologist at the Gladstone Institute of Cardiovascular Disease in San Francisco, California, who was not part of the study, says a daily treatment is best given as a pill, and proteins such as Tβ4 usually have to be delivered by injection.
Instead, he sees another possibility for the treatment. His group previously showed that treating mice with Tβ4 within hours of a heart attack helps muscle cells survive the injury. Srivastava and his co-workers are now working with RegeneRx Biopharmaceuticals of Rockville, Maryland, to test Tβ4 injections in humans, and the drug has already passed safety trials. The next phase of the drug trials might change in light of the new findings, which suggest that Tβ4 might continue to prime stem cells to make new cells after its initial survival effect has worn off. "Maybe we will inject for longer than 3 days," Srivastava says.
Although further experiments and clinical trials are needed to show whether Tβ4 works the same way in human hearts, and whether treatment is most effective before or after a heart injury, the scientists agree that self-repair is the best medicine for a broken heart.







