导读:美国研究人员指出,在心脏病发作时,病人体内的循环内皮细胞数量会显著增加,这一现象可以作为预测心脏病发作的新方法。但英国研究人员对研究结果的功效提出质疑。
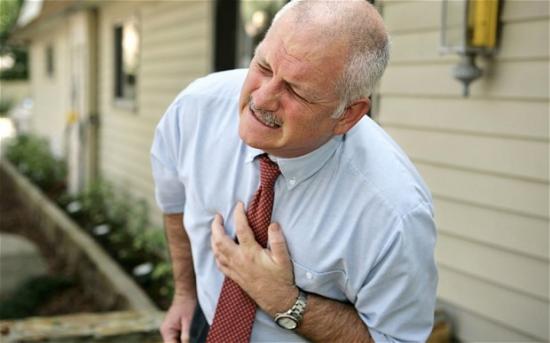
据英国《每日电讯报》网站3月21日报道,美国保健机构斯克利普斯健康的研究人员宣称,他们进行的一项研究表明,心脏病发作是可以预测的。这些研究人员指出,在心脏病发作前,患者动脉中的循环内皮细胞数量会大量增加。这也就是说,医生可以根据这一理论,预知心脏病患者的发病时间。
研究表明,在心脏病发作前数周,患者体内的循环内皮细胞很有可能会因为动脉破裂而被释放出来,导致血液中的该细胞数量骤增。随着循环内皮细胞数量的不断增加,这种具有警告性的现象将被医生察觉出来。目前,这项研究已经发表在美国《科学转化医学》杂志上,
研究人员指出,能够预知心脏病发作时间被誉为治疗心血管疾病的“最佳方法”,这种方法也使医生能够对急诊室中病患的病情予以判断。
在这项研究中,斯克利普斯健康机构的专家对50名心脏病人进行检测后发现,他们体内每毫升血液中含有的循环内皮细胞数量平均为12到51个,而正常人的含量大约是2到5个。
这项研究的带头人之一拉加夫·格拉普蒂博士说:“在急诊室中,这是判断病人是否马上或在未来两周内爆发心脏病的理想测量标准……目前,我们只能检测病人现在或以前是否经历过心脏病发作。因此,加上一些其他的检测数据,这种方法有望在未来一两年中投入商业使用。”
不过,斯克利普斯健康机构的这项研究引起一些英国专家的争议。这些专家指出,之前已经有多项欧洲研究得出了预知心脏病发作时间的方法,他们认为这些方法更为可靠。此外,他们还对美国最新研究结果的功效提出质疑。
伦敦大学学院心脏病专家约翰·马丁教授说:“我对任何在心脏病发作前进行抽血化验的预测方法深表质疑。同这项研究结果相比,血液循环中血小板聚集会导致心脏病发作这一说法的论据更有说服力,也是建立在更为可靠的原理之上的。”

 Characterization of Circulating Endothelial Cells in Acute Myocardial Infarction
Characterization of Circulating Endothelial Cells in Acute Myocardial Infarction
Samir Damani, Andrea Bacconi, Ondrej Libiger, Aparajita H. Chourasia, Rod Serry, Raghava Gollapudi, Ron Goldberg, Kevin Rapeport, Sharon Haaser, Sarah Topol, Sharen Knowlton, Kelly Bethel, Peter Kuhn, Malcolm Wood, Bridget Carragher, Nicholas J. Schork, John Jiang, Chandra Rao, Mark Connelly, Velia M. Fowler and Eric J. Topol
Acute myocardial infarction (MI), which involves the rupture of existing atheromatous plaque, remains highly unpredictable despite recent advances in the diagnosis and treatment of coronary artery disease. Accordingly, a clinical measurement that can predict an impending MI is desperately needed. Here, we characterize circulating endothelial cells (CECs) using an automated and clinically feasible CEC three-channel fluorescence microscopy assay in 50 consecutive patients with ST-segment elevation MI and 44 consecutive healthy controls. CEC counts were significantly elevated in MI cases versus controls, with median numbers of 19 and 4 cells/ml, respectively (P = 1.1 × 10−10). A receiver-operating characteristic (ROC) curve analysis demonstrated an area under the ROC curve of 0.95, suggesting near-dichotomization of MI cases versus controls. We observed no correlation between CECs and typical markers of myocardial necrosis (ρ = 0.02, creatine kinase–myocardial band; ρ = −0.03, troponin). Morphological analysis of the microscopy images of CECs revealed a 2.5-fold increase (P < 0.0001) in cellular area and a twofold increase (P < 0.0001) in nuclear area of MI CECs versus healthy controls, age-matched CECs, as well as CECs obtained from patients with preexisting peripheral vascular disease. The distribution of CEC images that contained from 2 to 10 nuclei demonstrates that MI patients were the only subject group to contain more than 3 nuclei per image, indicating that multicellular and multinuclear clusters are specific for acute MI. These data indicate that CEC counts may serve as a promising clinical measure for the prediction of atherosclerotic plaque rupture events.







