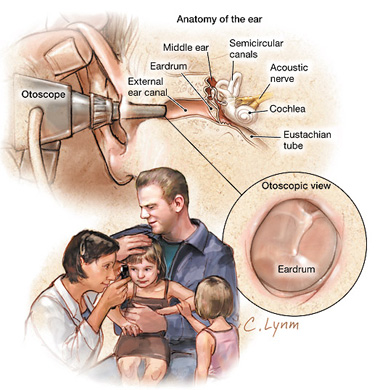
图片来源:美国医学会杂志网站
据11月17日刊《美国医学会杂志》上的一篇文章报道,在一项对儿童耳朵感染的以往的研究进行分析之后得到了各种发现,其中包括耳镜检查(这是一种对耳朵内进行检查的工具)的结果对做出准确诊断是至关重要的;而用抗菌素的效果比不用抗菌素治疗仅略微好些;大多数的抗菌素在正常风险的儿童中所取得的临床成功率很相似。
急性中耳炎(AOM)是儿童中最常见的感染。在美国,人们会开抗菌素处方来治疗中耳炎。一项用2006年的数据所做的研究显示,每位罹患中耳炎的孩子的平均医药费为350美元,该项花费的总额为28亿美元。文章的作者写道:“对中耳炎进行及时、精确的诊断及恰当的处理对流动门诊的使用及医疗开支会有明显的影响,… 然而,在诊断和治疗中存在着很大的差异。”
为了检查最近的试验结果和在临床做法中的变化,位于洛杉矶的加州大学洛杉矶分校David Geffen医学院的Tumaini R. Coker, M.D., M.B.A.及其同事对135项相关的研究进行了一个系统性的回顾以支持美国儿科协会的新的中耳炎治疗方针(目前正在准备之中)。
研究人员发现,耳镜检查所发现的鼓膜膨出和发红与疾病的精确诊断有关。他们写道:“也许改善诊断的最重要的方法是加强临床医生认识及依靠关键性耳镜发现的能力。”
文章的作者还发现,在少数可以得到的接种7价肺炎球菌结合疫苗(PCV7)前后的研究中,疫苗接种后的肺炎链球菌的流行率有所下降(例如:在中耳炎的分离物中,该细菌的流行率从33-48% 下降至23-31%),而流感嗜血杆菌的流行率则有所增加(从41-43% 上升至56-57%)。相对于安慰剂来说,立刻使用氨苄青霉素或阿莫西林可取得较高的短期临床成功率(73% vs. 60%),但皮疹或腹泻的发生率则从3%增加至5%。在4项研究中有2项显示,立刻使用抗菌素比延迟使用抗菌素有着更好的临床结果(分别为 95% vs. 80%及 86% vs. 70%)。
作者们写道:“在100名一般风险的中耳炎儿童中,如果不用抗菌素,大约有80名儿童可能会在约3天后病情好转。如果这些儿童全部给予即刻的氨苄青霉素/阿莫西林治疗的话,可能会有额外的12人的病情获得好转,但在这些人中,10个人中就可能有3人会出皮疹,10个人中会有5人出现腹泻。临床医生在对无并发症的中耳炎给予即刻的抗菌素治疗时,他们需要权衡这些风险(包括可能的对抗菌素抗药性的长期影响)和裨益。”
推荐英文摘要:
JAMA. 2010;304(19):2161-2169. doi:10.1001/jama.2010.1651
Diagnosis, Microbial Epidemiology, and Antibiotic Treatment of Acute Otitis Media in Children
Tumaini R. Coker, MD, MBA; Linda S. Chan, PhD; Sydne J. Newberry, PhD; Mary Ann Limbos, MD, MPH; Marika J. Suttorp, MS; Paul G. Shekelle, MD, PhD; Glenn S. Takata, MD, MS
Context Acute otitis media (AOM) is the most common condition for which antibiotics are prescribed for US children; however, wide variation exists in diagnosis and treatment.
Objectives To perform a systematic review on AOM diagnosis, treatment, and the association of heptavalent pneumococcal conjugate vaccine (PCV7) use with AOM microbiology.
Data Sources PubMed, Cochrane Databases, and Web of Science, searched to identify articles published from January 1999 through July 2010.
Study Selection Diagnostic studies with a criterion standard, observational studies and randomized controlled trials comparing AOM microbiology with and without PCV7, and randomized controlled trials assessing antibiotic treatment.
Data Extraction Independent article review and study quality assessment by 2 investigators with consensus resolution of discrepancies.
Results Of 8945 citations screened, 135 were included. Meta-analysis was performed for comparisons with 3 or more trials. Few studies examined diagnosis; otoscopic findings of tympanic membrane bulging (positive likelihood ratio, 51 [95% confidence interval {CI}, 36-73]) and redness (positive likelihood ratio, 8.4 [95% CI, 7-11]) were associated with accurate diagnosis. In the few available studies, prevalence of Streptococcus pneumoniae decreased (eg, 33%-48% vs 23%-31% of AOM isolates), while that of Haemophilus influenzae increased (41%-43% vs 56%-57%) pre- vs post-PCV7. Short-term clinical success was higher for immediate use of ampicillin or amoxicillin vs placebo (73% vs 60%; pooled rate difference, 12% [95% CI, 5%-18%]; number needed to treat, 9 [95% CI, 6-20]), while increasing the rate of rash or diarrhea by 3% to 5%. Two of 4 studies showed greater clinical success for immediate vs delayed antibiotics (95% vs 80%; rate difference, 15% [95% CI, 6%-24%] and 86% vs 70%; rate difference, 16% [95% CI, 6%-26%]). Data are absent on long-term effects on antimicrobial resistance. Meta-analyses in general showed no significant differences in antibiotic comparative effectiveness.
Conclusions Otoscopic findings are critical to accurate AOM diagnosis. AOM microbiology has changed with use of PCV7. Antibiotics are modestly more effective than no treatment but cause adverse effects in 4% to 10% of children. Most antibiotics have comparable clinical success.