2月27日,美国哥伦比亚大学医学中心科学家所领导的国际研究小组表示,他们利用实验鼠胚胎干细胞取代受损视网膜细胞,成功地帮助患色素性视网膜炎的实验鼠恢复了视力。该研究成果有望用于开发治疗人类色素性视网膜炎的新方法。
色素性视网膜炎在人类中的发病率为1/3000至1/4000,每年全球新增患者约150万人。人体视网膜色素上皮细胞是维持视觉能力的特殊细胞,色素性视网膜炎可导致视网膜周边的视觉细胞死亡,出现视觉变狭窄和四周模糊的“隧道视觉”病症。
该研究项目负责人、哥伦比亚大学医学中心眼科、病理学和细胞生物学副教授斯蒂芬曾表示,新的研究具有光明的前景,因为他们将干细胞转化成视觉细胞,帮助患病的实验鼠恢复了视力。他说,移植的细胞不仅外表像视觉细胞,而且其功能也与视觉细胞相当。
研究中,有1/4患病实验鼠在接受干细胞移植后视力得到恢复,但有些实验鼠出现了良性肿瘤和视网膜脱离的并发症。对此,斯蒂芬曾和同事表示,他们将进一步优化技术,以减少人类胚胎干细胞移植用于人体试验时并发症的发病率。
斯蒂芬曾表示,一旦并发症的问题得到解决,这将成为新的治疗方法,不仅能够医治色素性视网膜炎,而且还能治疗与年龄变老相关的视网膜黄斑变性、斯特格病变以及其他种类的视网膜疾病,它们均具有视网膜细胞损伤的特征。
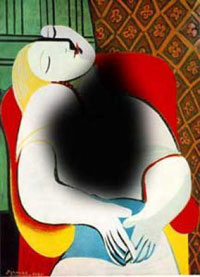
老年化视网膜黄斑变性患者眼中的图像
老年化视网膜黄斑变性是视网膜中心的视网膜细胞出现退化并导致视觉中心部分出现模糊的疾病。有研究表明,在美国,2010年将有900万人患上此种疾病,而2020年的发病率将是现在的两倍。年龄达75岁时,30%的人将患上某种类型的视网膜黄斑变性。
推荐原始出处:
Transplantation. 2010 Feb 15.
Transplantation of Reprogrammed Embryonic Stem Cells Improves Visual Function in a Mouse Model for Retinitis Pigmentosa
Wang NK, Tosi J, Kasanuki JM, Chou CL, Kong J, Parmalee N, Wert KJ, Allikmets R, Lai CC, Chien CL, Nagasaki T, Lin CS, Tsang SH.
1Department of Ophthalmology, Columbia University, New York City, NY. 2Department of Ophthalmology, Chang Gung Memorial Hospital, Linkou, Taiwan. 3Retina Division, Chang Gung University College of Medicine, Taoyuan, Taiwan. 4Department of Anatomy and Cell Biology, National Taiwan University, Taipei, Taiwan. 5Department of Genetics and Development, Columbia University, New York, NY. 6Institute of Human Nutrition, Columbia University, New York, NY. 7Department of Pathology and Cell Biology, Columbia University, New York, NY. 8Regenerative Medicine Division, Bernard and Shirlee Brown Glaucoma Laboratory, Columbia University, New York City, NY.
BACKGROUND.: To study whether C57BL/6J-Tyr/J (C2J) mouse embryonic stem (ES) cells can differentiate into retinal pigment epithelial (RPE) cells in vitro and then restore retinal function in a model for retinitis pigmentosa: Rpe65/Rpe65 C57BL6 mice. METHODS.: Yellow fluorescent protein (YFP)-labeled C2J ES cells were induced to differentiate into RPE-like structures on PA6 feeders. RPE-specific markers are expressed from differentiated cells in vitro. After differentiation, ES cell-derived RPE-like cells were transplanted into the subretinal space of postnatal day 5 Rpe65/Rpe65 mice. Live imaging of YFP-labeled C2J ES cells demonstrated survival of the graft. Electroretinograms (ERGs) were performed on transplanted mice to evaluate the functional outcome of transplantation. RESULTS.: RPE-like cells derived from ES cells sequentially express multiple RPE-specific markers. After transplantation, YFP-labeled cells can be tracked with live imaging for as long as 7 months. Although more than half of the mice were complicated with retinal detachments or tumor development, one fourth of the mice showed increased electroretinogram responses in the transplanted eyes. Rpe65/Rpe65 mice transplanted with RPE-like cells showed significant visual recovery during a 7-month period, whereas those injected with saline, PA6 feeders, or undifferentiated ES cells showed no rescue. CONCLUSIONS.: ES cells can differentiate, morphologically, and functionally, into RPE-like cells. Based on these findings, differentiated ES cells have the potential for the development of new therapeutic approaches for RPE-specific diseases such as certain forms of retinitis pigmentosa and macular degeneration. Nevertheless, stringent control of retinal detachment and teratoma development will be necessary before initiation of treatment trials.







