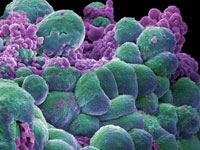
生物谷Bioon.net 讯 宾夕法尼亚大学医学院的研究人员开发了一种新颖的方法可攻击含有BRCA1或BRCA2基因变异的乳癌患者的肿瘤,能够减缓85%乳癌晚期患者的肿瘤生长,这项研究结果发布在7月6日的The Lancet杂志上。
这项研究的参与者Domchek教授表示,这是他们首次利用患者的遗传学原因,并将其作为靶标开发疗法。通常情况下研究会观察肿瘤本身的发展,然后尝试理解如何靶向定位肿瘤。在这项研究中,所有的患者都继承了BRCA1基因或BRCA2基因的变异,因此研究人员能够利用这一特点开发疗法,这种疗法或能减少对患者造成的副作用。提示:生物谷启用新域名www.bioon.net
所开发的新作用剂olaparib能够抑制一种叫PARP的蛋白。PARP和BRCA蛋白都参与DNA修复。细胞能够完成DNA修复只需其中的一个蛋白,然而当抑制缺乏BRCA基因的肿瘤中的PARP蛋白对于细胞来说很难承受,会致其死亡。
Domchek解释说:"如果给一个癌细胞施加太多的压力,它将不能承受并最终灭亡。因为继承有BRCA变异的患者中的非肿瘤细胞仍然保留BRCA基因的一个正常拷贝,所以相对来说他们不会受PARP抑制的影响。这类药物可能对肿瘤细胞具有强大杀伤力,且对正常细胞毒性更小,这对于癌症治疗来说是很重要的。
这项研究涉及54个患者,她们被平均分成两组。第一组27人每天两次每次均口服400毫克olaparib,第二组患者每天两次每次均口服100毫克olaparib。结果表明高剂量抑制剂似乎更具抵抗疾病的威力,在高剂量组中1位患者(4%)的肿瘤出现完全消退,10位患者(37%)表现出肿瘤明显减小,另外的12位患者(44%)表现出疾病稳定或肿瘤部分减小。在低剂量的一组,6位患者(22%)表现出明显肿瘤减小,12位患者(44%)肿瘤部分减小或保持稳定。
这项研究结果是令人兴奋的,但是在olaparib或其他PARP抑制剂进入常规使用前还需要进行一系列必要的临床研究。对于患者来说参加这些临床测试也是很重要的,可以确定更好的药物使用方式,即单独或联合用药,此外也需要最终确立这种抑制剂效果好于其他药物。
PARP抑制剂是癌症药物开发的重要变革,这是一种与众不同的癌症疗法。从肿瘤学角度来讲,这确实是首次在遗传易感性的基础上开发药物,这或将开辟一种药物开发的全新方式。
推荐原文出处:
The Lancet doi:10.1016/S0140-6736(10)60892-6
Oral poly(ADP-ribose) polymerase inhibitor olaparib in patients with BRCA1 or BRCA2 mutations and advanced breast cancer: a proof-of-concept trial
Dr Andrew Tutt PhD a , Mark Robson MD b, Judy E Garber MD c, Susan M Domchek MD d, M William Audeh MD e, Prof Jeffrey N Weitzel MD f, Prof Michael Friedlander PhD g, Prof Banu Arun MD h, Niklas Loman MD i, Prof Rita K Schmutzler MD j, Andrew Wardley MD k, Gillian Mitchell MD l, Helena Earl PhD m, Mark Wickens BSc n, Prof James Carmichael MD n
Background
Olaparib, a novel, orally active poly(ADP-ribose) polymerase (PARP) inhibitor, induced synthetic lethality in BRCA-deficient cells. A maximum tolerated dose and initial signal of efficacy in BRCA-deficient ovarian cancers have been reported. We therefore assessed the efficacy, safety, and tolerability of olaparib alone in women with BRCA1 or BRCA2 mutations and advanced breast cancer.
Methods
Women (aged ≥18 years) with confirmed BRCA1 or BRCA2 mutations and recurrent, advanced breast cancer were assigned to two sequential cohorts in a phase 2 study undertaken in 16 centres in Australia, Germany, Spain, Sweden, the UK, and the USA. The first cohort (n=27) was given continuous oral olaparib at the maximum tolerated dose (400 mg twice daily), and the second (n=27) was given a lower dose (100 mg twice daily). The primary efficacy endpoint was objective response rate (ORR). This study is registered with ClinicalTrials.gov, number NCT00494234.
Findings
Patients had been given a median of three previous chemotherapy regimens (range 1―5 in cohort 1, and 2―4 in cohort 2). ORR was 11 (41%) of 27 patients (95% CI 25―59) in the cohort assigned to 400 mg twice daily, and six (22%) of 27 (11―41) in the cohort assigned to 100 mg twice daily. Toxicities were mainly at low grades. The most frequent causally related adverse events in the cohort given 400 mg twice daily were fatigue (grade 1 or 2, 11 [41%]; grade 3 or 4, four [15%]), nausea (grade 1 or 2, 11 [41%]; grade 3 or 4, four [15%]), vomiting (grade 1 or 2, three [11%]; grade 3 or 4, three [11%]), and anaemia (grade 1 or 2, one [4%]; grade 3 or 4, three [11%]). The most frequent causally related adverse events in the cohort given 100 mg twice daily were nausea (grade 1 or 2, 11 [41%]; none grade 3 or 4) and fatigue (grade 1 or 2, seven [26%]; grade 3 or 4, one [4%]).
Interpretation
The results of this study provide positive proof of concept for PARP inhibition in BRCA-deficient breast cancers and shows a favourable therapeutic index for a novel targeted treatment strategy in patients with tumours that have genetic loss of function of BRCA1-associated or BRCA2-associated DNA repair. Toxicity in women with BRCA1 and BRCA2 mutations was similar to that reported previously in those without such mutations.







