最近美国杜克大学医学院利用诱导多能干细胞(iPSCs)成功地在小鼠实验中培育出软骨,可用于修复组织、研究软骨损伤和骨关节炎病症等。研究人员认为,iPSCs有望成为病人专用人造软骨组织的来源。相关论文在线发表于10月29日的美国《国家科学院学报》上。
论文作者、杜克医学院整形外科手术教授法希德·盖拉克介绍说,iPSCs的技术能将成熟干细胞转化,使其具有胚胎干细胞的属性,可以实现无限供给,并能变成任意类型的组织。“我们这次成功让iPSCs发育成没有再生能力的软骨。”

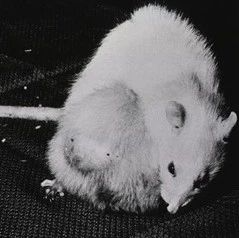
由于iPSCs功能强大,实验中需要克服一个难题,让其发育成完全一致的软骨细胞,能产生胶原蛋白并维持软骨,同时要剔除iPSCs可能形成的其他类型细胞。为此,研究人员从成年小鼠的成纤维细胞中采集iPSCs,用生长物质处理培养,诱导它们分化为软骨细胞。他们还将软骨细胞特制成能表达绿色荧光蛋白的细胞,一旦iPSCs成功变成了软骨细胞,就会发出绿色荧光,从而很容易将软骨细胞和其他细胞区别开来。特制细胞也能产生胶原蛋白等更多的软骨成分,并表现出天然软骨特有的硬度,这表明它们在修复身体软骨缺陷方面非常有效。
关节软骨是关节中的一种减震组织,让人们在行走、爬楼梯、跳跃以及日常活动中避免疼痛。但日常磨损和外伤会降低保护效果,还可能发展成骨关节炎。由于关节软骨的修复能力很差,所以骨损伤和骨关节炎也是老年病的主要原因,甚至需要更换关节。
研究人员表示,下一步将用人类iPSCs来培育软骨。“目前对骨关节炎还没有治愈的方法,也没有遏制软骨耗损的有效疗法。”盖拉克说,“除用于细胞疗法,iPSCs技术还能为病人提供个体专用的细胞和组织模型,筛选治疗骨关节炎的药物等。”
用干细胞培养的人体组织,是最有希望的器官移植来源。而制造出天然骨骼和皮肤,是未来最可能率先突破的领域。关节软骨是非常容易磨损的组织,结构简单,如果有软骨组织供应,移植手术很容易成功。但这样简单的组织,人们也无法原样复制,直到有了干细胞技术。一旦软骨复制方法成熟,今后关节炎和关节运动损伤,将会像白内障一样容易根治。

Cartilage tissue engineering using differentiated and purified induced pluripotent stem cells
Brian O. Diekman, Nicolas Christoforou, Vincent P. Willard, Haosi Sun, Johannah Sanchez-Adams, Kam W. Leong, and Farshid Guilak
The development of regenerative therapies for cartilage injury has been greatly aided by recent advances in stem cell biology. Induced pluripotent stem cells (iPSCs) have the potential to provide an abundant cell source for tissue engineering, as well as generating patient-matched in vitro models to study genetic and environmental factors in cartilage repair and osteoarthritis. However, both cell therapy and modeling approaches require a purified and uniformly differentiated cell population to predictably recapitulate the physiological characteristics of cartilage. Here, iPSCs derived from adult mouse fibroblasts were chondrogenically differentiated and purified by type II collagen (Col2)-driven green fluorescent protein (GFP) expression. Col2 and aggrecan gene expression levels were significantly up-regulated in GFP+ cells compared with GFP− cells and decreased with monolayer expansion. An in vitro cartilage defect model was used to demonstrate integrative repair by GFP+ cells seeded in agarose, supporting their potential use in cartilage therapies. In chondrogenic pellet culture, cells synthesized cartilage-specific matrix as indicated by high levels of glycosaminoglycans and type II collagen and low levels of type I and type X collagen. The feasibility of cell expansion after initial differentiation was illustrated by homogenous matrix deposition in pellets from twice-passaged GFP+ cells. Finally, atomic force microscopy analysis showed increased microscale elastic moduli associated with collagen alignment at the periphery of pellets, mimicking zonal variation in native cartilage. This study demonstrates the potential use of iPSCs for cartilage defect repair and for creating tissue models of cartilage that can be matched to specific genetic backgrounds.
文献链接:https://www.pnas.org/content/early/2012/10/30/1210422109.abstract