许多至关重要的细胞功能取决于一种被称为嘌呤的分子,嘌呤分子是DNA和RNA的主要组成部分,也是细胞储存能量物质的主要成分。细胞严格控制嘌呤的供应,任何破坏都会有严重的后果。
最新一项研究,麻省理工的生物工程师精确地测量了嘌呤合成和分解过程中出现错误的影响。他们发现当一种酶用于调节嘌呤合成和分解过程缺乏时,竟会改变一个细胞的DNA序列。研究成果发表在1月30日出版的Proceedings of the National Academy of Sciences 杂志上。
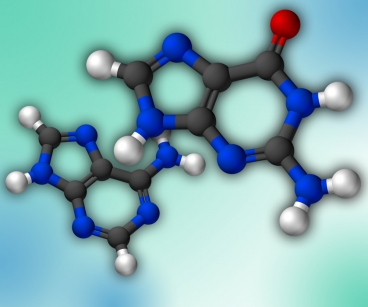
DNA通常是由四种核苷酸组成:腺嘌呤,鸟嘌呤,胞嘧啶和胸腺嘧啶(即A、G、C、T组成密码子)。鸟嘌呤和腺嘌呤都是嘌呤类,每种嘌呤都有结构相近,可以在DNA或 RNA合成中代替其位置的化合物,当这些核苷酸比如黄嘌呤和次黄嘌呤错误的嵌入DNA中,便会导致突变。它们会影响信使RNA(mRNA)的功能,信使RNA携带DNA的结构到细胞的其他地方,同时也会影响将mRNA翻译成蛋白质的RNA分子。
“细胞需要小心控制核苷酸的分配,从而保证在合成DNA时,几种核苷酸的数量正确。如果细胞在分配这些核苷酸有所失衡,这就会导致错误的发生。” Peter Dedon教授说,他是麻省理工学院的生物工程师,也是这项研究的高级作者。
嘌呤除了形成DNA和RNA的主要组成部分,还是细胞“能量货币”ATP的主要化合物;其他分子则管理着细胞的能量流;而几千种细胞酶的活性则需要各种小的化学辅因子。
许多酶都参与嘌呤的新陈代谢,而且人们也知道这些酶出现故障时会有副作用。比如说,当调控DNA和RNA分解中回收嘌呤核苷酸的补救酶缺失时,就会导致血液中尿酸浓度增高,从而引发痛风和肾结石——在极端的案例中,会出现一种神经学上的紊乱被称作莱希—尼亨综合症。缺失另一种补救酶会导致一种被称为重症联合免疫缺陷的疾病。
异常的嘌呤代谢同样会对服用thiopurines的人产生副作用。对于一些患者,这些药物也被用来治疗白血病、淋巴瘤、克罗恩病、风湿性关节炎以及器官移植排斥等,然而这些药物会代谢产生一些有毒的化合物。基因检测能够显示哪些病人需要避免thiopurines这类药物。
在这项新研究中,Dedon和他的同事破坏了大肠杆菌和酵母菌一半的嘌呤代谢酶。修改了这些酶后,研究人员通过一种高度敏感的质谱分析法技术检测了合成DNA和RNA的黄嘌呤和次黄嘌呤数量,他们先前通过这项技术已经研究了炎症引起的DNA和RNA损伤。他们发现有问题的酶能够导致惊人的增长,代替腺嘌呤合成DNA和RNA的次黄嘌呤数量多了1000倍。然而原鸟嘌呤位置的黄嘌呤数量变化很小。
俄勒冈州大学退休的生物化学和生物物理学家Chris Mathews教授,说这项发现有助于研究人员更好的理解嘌呤代谢错误如何导致疾病。
科学家已经发现一些人类嘌呤代谢酶中的基因突变,所以这个研究小组计划调查这些基因突变对嵌入DNA和RNA的黄嘌呤和次黄嘌呤的影响。他们也对DNA的另两种核苷酸即胞嘧啶和胸腺嘧啶的代谢感兴趣。

Defects in purine nucleotide metabolism lead to substantial incorporation of xanthine and hypoxanthine into DNA and RNA
Bo Pang, Jose L. McFaline, Nicholas E. Burgis, Min Dong, Koli Taghizadeh, Matthew R. Sullivan, C. Eric Elmquist, Richard P. Cunningham, and Peter C. Dedon
Deamination of nucleobases in DNA and RNA results in the formation of xanthine (X), hypoxanthine (I), oxanine, and uracil, all of which are miscoding and mutagenic in DNA and can interfere with RNA editing and function. Among many forms of nucleic acid damage, deamination arises from several unrelated mechanisms, including hydrolysis, nitrosative chemistry, and deaminase enzymes. Here we present a fourth mechanism contributing to the burden of nucleobase deamination: incorporation of hypoxanthine and xanthine into DNA and RNA caused by defects in purine nucleotide metabolism. Using Escherichia coli and Saccharomyces cerevisiae with defined mutations in purine metabolism in conjunction with analytical methods for quantifying deaminated nucleobases in DNA and RNA, we observed large increases (up to 600-fold) in hypoxanthine in both DNA and RNA in cells unable to convert IMP to XMP or AMP (IMP dehydrogenase, guaB; adenylosuccinate synthetase, purA, and ADE12), and unable to remove dITP/ITP and dXTP/XTP from the nucleotide pool (dITP/XTP pyrophosphohydrolase, rdgB and HAM1). Conversely, modest changes in xanthine levels were observed in RNA (but not DNA) from E. coli lacking purA and rdgB and the enzyme converting XMP to GMP (GMP synthetase, guaA). These observations suggest that disturbances in purine metabolism caused by known genetic polymorphisms could increase the burden of mutagenic deaminated nucleobases in DNA and interfere with gene expression and RNA function, a situation possibly exacerbated by the nitrosative stress of concurrent inflammation. The results also suggest a mechanistic basis for the pathophysiology of human inborn errors of purine nucleotide metabolism.








